Project Management is not all about being cost-effective; sometimes, it literally saves lives. In 2013, the Journal of Patient Safety reported that over 210,000 deaths1 annually in the U.S. were linked to preventable medical errors—often the result of mismanaged projects and poor communication.
One infamous case involved a botched EHR system implementation2, which made critical patient data inaccessible in emergencies. The cost? Lives lost, lawsuits filed, and millions in financial damages.
In this blog, we’ll explore how effective project management can be the difference between success and catastrophic failure in healthcare.
Let’s dive in!
What Is Healthcare Project Management?
Healthcare project management involves applying structured methodologies and tools to tackle the unique challenges of healthcare initiatives, such as regulatory compliance, stakeholder coordination, and safeguarding patient data. Whether implementing an Electronic Health Record (EHR) system or expanding a hospital, effective project management is essential for mitigating risks, controlling budgets, and improving patient outcomes.
Managing Stakeholders: Healthcare projects typically involve diverse stakeholders, including clinical staff, IT teams, administrators, and regulatory bodies. You should use tools like a RACI matrix (Responsible, Accountable, Consulted, Informed) to clarify roles and responsibilities to align their often-conflicting priorities. Regular stakeholder meetings and tailored communication strategies help ensure everyone remains aligned with project goals.
Regulatory Compliance: Adherence to regulations like HIPAA and HITECH is non-negotiable. To ensure compliance throughout the project lifecycle, managers can integrate compliance management software that tracks regulatory requirements in real-time. Implementing checklists and conducting regular audits are essential for identifying gaps early on. Failure to comply with these regulations can lead to costly penalties and reputational damage.
Risk Mitigation: Healthcare projects are prone to scope creep and delays, with over 90% facing budget or timeline overruns3. To counter this, project managers should establish a risk register at the outset, listing potential risks and corresponding mitigation strategies.
Additionally, setting aside a contingency reserve and conducting regular risk assessments ensures preparedness for unforeseen challenges.
Improving Patient Outcomes: Ultimately, healthcare project management must focus on improving patient care. For instance, using Lean principles can reduce patient wait times and enhance operational efficiency, directly impacting patient satisfaction and safety.
You should align project goals with measurable outcomes, such as reducing hospital readmissions or improving recovery times.
Why Do You Need Healthcare Project Management?
Healthcare project management is essential for improving patient care, controlling rising costs, and ensuring compliance with strict regulatory standards.
Improved Patient Care

Effective project management directly impacts patient outcomes by streamlining workflows and ensuring that projects—such as Electronic Health Record (EHR) implementations or new treatment protocols—are delivered on time and without disruptions.
Research shows that when healthcare organizations apply methodologies like Agile or Lean, they can reduce patient wait times and improve care coordination, resulting in higher patient satisfaction and better health outcomes. For example, Lean principles have helped hospitals reduce waste, minimize wait times, and optimize patient flow.
Cost Control
One of the major challenges in healthcare is managing costs, which continue to escalate year over year. Without efficient project management, healthcare organizations often face budget overruns and missed deadlines.
In fact, poorly managed projects can increase costs by as much as 20%4. By implementing regular cost tracking, using Gantt charts for timeline management, and applying Lean methodologies, project managers can keep projects within budget and even identify areas for cost savings, such as reducing unnecessary resource usage.
Regulatory Compliance

Healthcare is one of the most heavily regulated industries, with regulations such as HIPAA in the U.S. and GDPR in Europe governing data privacy and patient safety.
According to the American Hospital Association, the average community hospital spends over $7.5 million annually on regulatory compliance5. Non-compliance can lead to severe financial penalties and reputational damage.
Effective project management ensures that regulatory compliance is built into every project phase, from planning to execution, by using tools like compliance tracking software and real-time audits to avoid costly mistakes.
Core Components of Healthcare Project Management
Project Definition and Scope
Defining the project scope in healthcare is essential to avoid common pitfalls like scope creep, leading to cost overruns and missed deadlines. A well-crafted project charter should clearly outline the objectives, deliverables, timelines, and resources necessary for the project.
For example, when managing an Electronic Health Record (EHR) system implementation, the scope must define which clinical workflows will be integrated, which patient records are prioritized for digitization, and the security protocols needed for compliance.
Managing Scope Creep
Research shows that 49% of completed projects6 experience scope creep, leading to up to 20% budget increases in some cases. This is especially critical in healthcare, where mid-project regulatory changes (such as updates to HIPAA or data security laws) can disrupt workflows.
To manage this, project managers must implement a change control board (CCB) to review any changes and assess their impact on the project. Regular scope reviews and stakeholder alignment meetings can help prevent minor changes from snowballing into costly disruptions.
Additionally, tools like Microsoft Project allow you to track project scope in real time, ensuring that any deviations are flagged and addressed early. Techniques like Earned Value Management (EVM) can also be deployed to monitor how scope changes affect cost and schedule performance, providing a clear snapshot of project health.
Resource Allocation and Management
Effective resource allocation is critical in healthcare project management due to the complex and fluctuating demands on staff and physical resources. Managing resources in a clinical setting requires balancing doctor and nurse availability and aligning department-specific resources to meet patient needs.
Fluctuations in patient volume, unexpected staff absences, or changing regulatory requirements make this even more challenging. For instance, resource shortages severely disrupt patient care during high-demand periods like flu season or a pandemic surge.
Strategies: One key strategy is conducting a thorough resource needs assessment that considers historical data on patient demand and staff availability. Tools like capacity planning software allow healthcare administrators to forecast staffing needs and make adjustments in real time.
Implementing centralized scheduling systems for doctors and nurses can optimize resource allocation and prevent burnout by balancing workloads. This system can help reduce errors caused by overburdened staff and improve the quality of patient care.
Risk Assessment and Mitigation

Effective risk management in healthcare requires a proactive approach to identify, assess, and mitigate risks. Key risks include patient safety concerns, regulatory non-compliance, and financial overspending.
For example, medication errors alone contribute to nearly 400,000 deaths annually in the U.S., with an associated financial burden of $42 billion7.
Additionally, healthcare organizations spend an average of $7.6 million8 annually to maintain regulatory compliance. These figures emphasize the importance of a robust risk management process.
Step-by-Step Framework for Risk Management
- Risk Identification: Conduct a comprehensive risk identification exercise involving all stakeholders, including clinicians, administrators, and compliance officers. Use risk prompt lists and past project data to ensure all risks are captured.
- Risk Register Creation: Document identified risks in a risk register, detailing the likelihood of occurrence, potential impact, and mitigation strategies for each risk. The risk register should be updated regularly and reviewed during project meetings.
- Continuous Monitoring: Implement real-time monitoring tools such as compliance management software (e.g., Microsoft Compliance Manager, IBM QRadar) to track adherence to regulations like HIPAA. Integrating compliance tools helps ensure regulatory requirements are met throughout the project lifecycle.
Mitigation Strategies
- Using Risk Matrices: A risk matrix is an effective tool to visualize and prioritize risks based on their likelihood and impact. Project managers can focus resources on high-priority risks, such as potential regulatory breaches or patient safety issues.
- Root Cause Analysis (RCA): After a risk materializes (e.g., a medication error), conduct a Root Cause Analysis (RCA) to determine the underlying cause and prevent recurrence. RCA is particularly effective in addressing patient safety risks by identifying systemic failures in clinical processes.
Ensuring Compliance: In healthcare, compliance with regulations is non-negotiable. Tools like Microsoft Compliance Manager or IBM QRadar help automate compliance tracking, providing real-time monitoring of regulatory changes. These tools enable healthcare organizations to stay ahead of audits and avoid costly fines.
Stakeholder Engagement
Effective stakeholder engagement is essential for healthcare project management, where interdisciplinary collaboration is critical. Projects often involve clinical staff, administrative teams, and IT departments, all with unique objectives and priorities. Managing these diverse groups requires clear communication, well-defined roles, and a structured approach to decision-making.
Interdisciplinary Collaboration
Healthcare projects require balancing the needs of various departments. Clinical teams focus on patient care, administrative staff ensure compliance and resource allocation, and IT supports the technology infrastructure.
Ensuring these groups work together seamlessly is essential. One effective technique is holding regular interdisciplinary meetings where stakeholders can raise concerns and share updates.
Assigning a project manager to facilitate these discussions ensures that every department’s needs are considered and helps prevent misunderstandings that could delay the project.
RACI Matrix for Clarity
The RACI matrix (Responsible, Accountable, Consulted, Informed) is valuable for ensuring clarity and accountability across departments. By mapping out roles and responsibilities, it helps avoid role confusion and duplication of efforts.
For example, in a hospital IT project, clinical staff may be “Consulted” for system requirements, while the IT department is “Responsible” for implementation, and the hospital administration remains “Informed” throughout.
Using a RACI matrix in complex healthcare projects enhances communication and ensures all stakeholders understand their responsibilities, leading to more efficient collaboration and decision-making.
Quality Assurance

In healthcare project management, quality assurance (QA) is not just about completing projects on time—it’s about ensuring every aspect of the project meets stringent healthcare quality standards that safeguard patient safety and clinical effectiveness.
This involves adhering to protocols, guidelines, and standards such as ISO 9001 and Total Quality Management (TQM), which emphasize continuous improvement across clinical, administrative, and IT teams.
Step-by-Step Guide to Implementing QA
- Conduct a Gap Analysis: Start by identifying gaps between current practices and industry standards. This analysis helps project managers understand where improvements are needed, particularly in patient safety protocols and compliance with healthcare regulations like HIPAA.
- Develop a Corrective Action Plan: Once gaps are identified, project managers must create a Corrective Action Plan (CAP) that outlines steps to resolve deficiencies. This plan should address clinical workflows, technology integration, and patient data security.
- Implement Regular Audits: Conduct regular audits to track adherence to quality standards and identify potential risks. These audits should be both internal and external to ensure thorough oversight. Audits have been shown to improve compliance with safety protocols by up to 30%9.
- Continuous Review and Feedback: QA doesn’t end with audits. Project managers must establish a continuous review process involving all stakeholders to ensure that corrective actions are implemented effectively and to adjust the strategy as needed.
Healthcare-Specific Tools for QA
- Statistical Process Control (SPC): This tool is used to monitor critical metrics such as patient wait times or surgical outcomes, ensuring that processes remain within acceptable ranges. SPC helps healthcare teams identify and address issues before they escalate.
- Failure Mode and Effects Analysis (FMEA): FMEA is ideal for healthcare projects where patient safety is paramount. It helps project managers anticipate potential failures in processes (e.g., medication distribution) and implement preventive measures to avoid adverse outcomes.
Real-Time Monitoring: In today’s fast-paced healthcare environment, real-time data monitoring is essential. Using quality dashboards or automated systems, healthcare project managers can track critical clinical and operational metrics in real time. These tools allow for immediate adjustments to processes, improving response times and reducing risks.
Adherence to Regulations
In healthcare, regulatory compliance is essential to ensure that all processes meet the required safety, security, and ethical standards. Key laws such as HIPAA (Health Insurance Portability and Accountability Act), FDA regulations for medical devices, and GDPR (General Data Protection Regulation) for patient data protection mandate stringent controls over patient information, medical procedures, and product safety.
Steps to Ensure Compliance:
- Establish a Compliance Program: Healthcare organizations must have a structured compliance program with clear policies and guidelines tailored to HIPAA, FDA, and GDPR requirements. Appointing a compliance officer and conducting regular staff training ensures everyone is up-to-date with the latest regulatory demands.
- Risk Assessments and Audits: It is critical to conduct regular risk assessments to identify potential gaps in compliance. Periodic audits, both internal and external, should ensure that all operational processes, including data handling, meet the legal requirements. For example, non-compliance with HIPAA can result in fines of up to $1.5 million per violation per year10, while GDPR violations can reach up to €20 million or 4% of global revenue.
- Data Security and Privacy: Strong cybersecurity measures are crucial, with patient data increasingly digitized. Encryption, access controls, and secure data storage are essential to comply with HIPAA and GDPR. Healthcare project managers must ensure patient data is protected throughout the project lifecycle.
Regulatory Change Management: Healthcare regulations frequently evolve, and staying compliant requires an adaptive approach. Project managers should establish real-time tracking mechanisms for regulatory updates and ensure rapid response protocols are in place.
For example, when HIPAA or FDA regulations are updated, swift action is required to update internal policies, retrain staff, and potentially modify technology systems.
Change Management
In healthcare, managing change is often met with resistance, making it essential to involve clinicians and administrators early in the process. Whether implementing new technology or shifting clinical procedures, engaging key stakeholders from the outset helps align goals and smooth the transition.
Healthcare-Specific Change Management Frameworks
Involving clinical staff and administrators is crucial to managing resistance. Early participation fosters buy-in and ensures that concerns are addressed before they evolve into obstacles.
This engagement can be facilitated through regular meetings, workshops, and pilot projects that allow all stakeholders to voice their concerns and contribute to the planning process. By involving staff directly impacted by the change—like doctors, nurses, and IT personnel—you ensure that the practicalities of daily operations are considered, minimizing disruptions during the transition.
Applying the ADKAR Model
The ADKAR model (Awareness, Desire, Knowledge, Ability, Reinforcement) provides a structured approach to healthcare change management, guiding individual and organizational transitions. Here’s how ADKAR can be applied:
- Awareness: Start by communicating the need for change. For instance, if you’re rolling out a new electronic health records (EHR) system, explain how it will improve patient care by reducing errors and increasing efficiency.
- Desire: Build desire by sharing success stories from similar projects. Highlight case studies where hospitals saw improved patient outcomes and streamlined operations after implementing EHR systems.
- Knowledge: Train staff to use the new system effectively. Offer hands-on training sessions to ensure they understand both the technical aspects and the impact on patient care.
- Ability: Offer continuous support during the transition to enable staff to apply what they’ve learned. For example, provide a dedicated helpdesk or peer mentors who can troubleshoot issues as they arise.
- Reinforcement: Ensure long-term success by monitoring the adoption of new processes and celebrating small wins. Track metrics like reduced patient wait times or fewer medication errors, reinforcing the positive outcomes of the change.
Post-Implementation Evaluation
Evaluating the success of a healthcare project doesn’t stop at its completion. Post-implementation evaluation is critical for ensuring the project meets its original objectives and delivers tangible benefits, such as improved patient outcomes and operational efficiencies.
In healthcare, this requires a focus on specific Key Performance Indicators (KPIs) that align with both clinical and administrative goals.
Specific Healthcare KPIs
- Patient Satisfaction Scores: This KPI reflects how well the healthcare facility meets patient needs and expectations. Tracking patient satisfaction is vital for assessing the quality of care and identifying areas for improvement. Facilities using satisfaction surveys have seen up to 15% improvement in patient feedback11 after implementing changes.
- Hospital Readmission Rates: A critical measure of care quality, hospital readmission rates evaluate how many patients return to the hospital within a specific time frame after discharge. Reducing readmission rates improves patient outcomes and lowers costs associated with repeated treatments.
- Cost Savings: Monitoring cost savings helps quantify the project’s financial impact. Efficient resource management reduces patient wait times, and improved workflow efficiency can significantly reduce operating expenses.
- Adherence to Regulatory Timelines: It is essential to ensure that the project adheres to all regulatory deadlines, such as those related to HIPAA or FDA compliance. Failure to meet these timelines can result in penalties and negatively affect project success.
Tools for Performance Tracking: To effectively track these KPIs, healthcare project managers can leverage dashboards and data analytics tools. Dashboards provide real-time visibility into critical metrics, such as patient satisfaction, readmission rates, and cost savings, helping managers make informed decisions quickly.
Popular Healthcare Project Management Methodologies
Waterfall Methodology
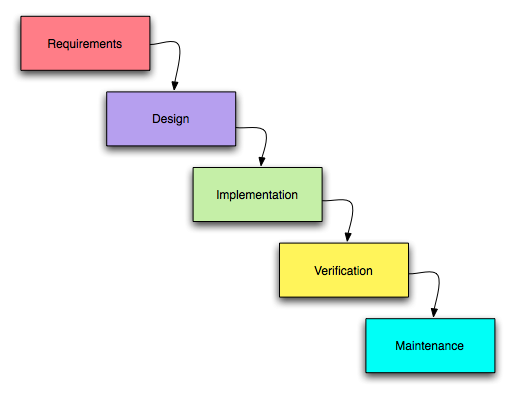
The Waterfall methodology is most effective for healthcare projects with rigid regulatory and compliance requirements, such as hospital construction or medical device implementation. Each phase in these projects— planning, design, and execution—must be completed before the next phase begins.
For example, in a hospital construction project, you would finalize architectural plans and obtain regulatory approvals before starting construction, ensuring that every step meets FDA regulations or local building codes. This structured approach reduces risks of non-compliance and cost overruns.
Step-by-Step Application:
- Initiation: Define the project scope and gather regulatory requirements.
- Planning: Develop detailed timelines using tools like Gantt charts to manage project phases.
- Execution: Implement each stage, ensuring that inspections and approvals are obtained at the appropriate milestones.
- Closeout: Complete final reviews and ensure all compliance standards are met before project handoff.
Agile Methodology
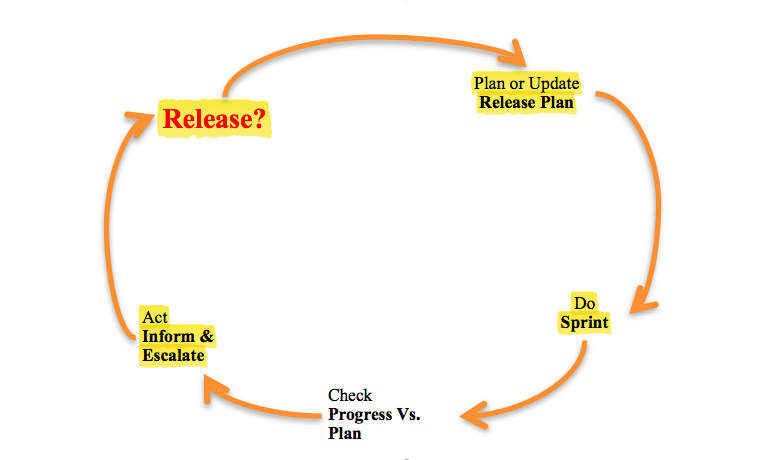
The Agile methodology is ideal for projects that need flexibility and iterative feedback, such as telehealth implementation or EHR system development. Agile thrives in dynamic environments, enabling continuous improvement through short development cycles known as sprints.
For instance, during a telehealth system rollout, Agile allows for rapid user feedback from doctors and patients, so adjustments can be made without delaying the overall project. This adaptability is crucial in healthcare IT, where user needs and regulatory requirements change frequently.
Steps in Agile
- Sprint Planning: Break down the project into short, manageable sprints, each focusing on developing a specific feature.
- Daily Standups: Hold brief, daily check-ins to ensure teams are aligned and issues are addressed promptly.
- Sprint Reviews: After each sprint, gather user feedback and implement necessary changes before starting the next development phase.
Hybrid Methodology
The Hybrid methodology blends Waterfall’s structured approach with Agile’s flexibility, making it ideal for complex healthcare projects like hospital expansion combined with IT systems integration. For example, the construction phase of a hospital expansion would follow Waterfall to ensure compliance with building regulations, while the IT systems integration could use Agile for iterative development and testing of healthcare software. This method provides the stability needed for regulatory tasks while allowing adaptability for technology updates.
Real-World Case: IBM 12successfully implemented a hybrid model in healthcare IT, using Agile for software development and Waterfall for regulatory approvals. This allowed for faster software delivery while maintaining compliance with healthcare standards.
How to Integrate Project Management in Your Healthcare Organization
| Step | Description | Example/Tools |
| 1. Conduct Organizational Assessment | Assess the current state of project management capabilities in the organization. Identify gaps in process, communication, and regulatory compliance to create a roadmap for improvements. | Conduct audits of current processes and use gap analysis techniques. |
| 2. Define Governance and Roles | Establish a governance structure, assigning roles and responsibilities across departments. Clarity in leadership and accountability is key for project success. | Create a Project Management Office (PMO) to centralize oversight. Assign roles using RACI matrices. |
| 3. Set Objectives and KPIs | Define measurable goals for project management integration. Use KPIs like project completion rates, budget adherence, and compliance with regulations. | KPIs: Completion rates, budget adherence, staff satisfaction, regulatory compliance. |
| 4. Stakeholder Engagement | Engage key stakeholders (clinicians, administrators, IT) from the beginning to ensure alignment and reduce resistance. | Cross-departmental workshops to gather feedback, RACI matrices for role clarity. |
| 5. Track KPIs | Regularly monitor performance using KPIs to ensure the integration process is successful. Adjust strategies based on findings from these metrics. | KPIs: On-time project delivery, budget adherence, staff engagement surveys, regulatory compliance monitoring. |
How to Stay Compliant as a Healthcare Project Manager

Staying compliant with HIPAA, GDPR, and other healthcare regulations is a core responsibility for healthcare project managers. Non-compliance risks include significant fines, security breaches, and damage to patient trust. Here’s how to ensure compliance through practical, actionable steps:
1. Perform Detailed Risk Assessments
Start by conducting a thorough HIPAA-compliant risk assessment for every project phase, from initiation to completion. Follow the NIST 800-66 guidelines, which help healthcare organizations identify and manage risks to Protected Health Information (PHI). Here’s how to structure your risk assessment:
- Identify vulnerabilities: Evaluate how PHI is accessed, transmitted, and stored.
- Prioritize risks: Use a risk matrix to categorize risks based on severity and likelihood.
- Mitigation strategies: Develop action plans to minimize each risk.
- Follow-up assessments: Conduct reviews at key project milestones to ensure risks remain under control. A study showed that healthcare organizations that regularly assess risk have 30% fewer data breaches than those that don’t.
2. Leverage Compliance Tools
Strong data security protocols are non-negotiable in healthcare. Implement encryption for all PHI, both in transit and at rest. Use specialized compliance tools like:
- HIPAA One: Automates risk assessments, workflow management, and auditing for HIPAA compliance.
- Vanta: Provides continuous monitoring and security alerts for HIPAA and GDPR.
- Tugboat Logic: Helps organizations maintain compliance by automating audits and managing security risks. By integrating these tools, project managers can reduce the risk of non-compliance and data breaches, which can cost healthcare organizations an average of $9.23 million per breach13.
3. Real-Time Compliance Monitoring
Healthcare regulations are complex and change frequently, so real-time monitoring is essential. Use compliance dashboards that track security incidents, potential violations, and access logs.
Tools like Splunk can integrate real-time alerts and dashboards to provide immediate visibility into compliance issues, helping project managers react quickly. This proactive approach is critical in preventing incidents before they escalate into violations.
4. Ensure Vendor Compliance
Third-party vendors are often weak links in compliance efforts. Ensure that all vendors handling patient data sign Business Associate Agreements (BAAs) and undergo rigorous security audits.
Studies show that 60% of healthcare breaches14 originate from third-party vendors. Regularly review and audit vendor processes to ensure they meet the same compliance standards as your organization.
5. Ongoing Training and Regulatory Updates
Continuous education is critical for keeping your team compliant. Develop a security awareness program that covers HIPAA guidelines, data handling practices, and phishing attack prevention.
Studies show that ongoing security training reduces human error-based violations by 70%15. Additionally, establish a regulatory monitoring system that automatically sends updates on changes from agencies like HHS or the FDA, ensuring swift responses to new requirements.
Real-World Example
One major hospital network implemented continuous training and vendor management, reducing HIPAA violations by 50%16 and avoiding costly fines. By regularly auditing third-party vendors and using compliance dashboards to monitor real-time risks, the hospital successfully maintained full regulatory compliance during a system-wide EHR upgrade.
Metrics and Performance Tracking in Healthcare Projects
| Metric/Tool | Description | Importance in Healthcare |
| Patient Satisfaction Scores | Measures how well healthcare services meet patient expectations and needs. | Higher patient satisfaction is linked to better care outcomes and fewer malpractice claims. |
| Readmission Rates | Tracks the percentage of patients readmitted to the hospital after discharge. | Reducing readmission rates improves care quality and lowers rehospitalization costs. |
| Project Completion Times | Measures project duration relative to planned timelines. | Ensures timely project delivery, minimizing disruptions in patient care and operations. |
| Budget Adherence | Monitors how well projects stay within their allocated budgets. | Helps avoid cost overruns and ensures resource availability for patient care. |
| Performance Tracking Tools | Tools like ClearPoint Strategy and Domo track KPIs in real time. | Real-time dashboards enable data-driven decisions and trend identification. |
Real-Life Case Studies of Healthcare Projects
1. The Everett Clinic EHR Implementation
At the Everett Clinic in Washington state, transitioning from paper records to an EHR system improved care delivery and significantly reduced time spent documenting patients. The system reduced documentation time by 15%, allowing clinicians to focus more on patient care.
Additionally, administrative errors decreased by 20%, leading to a reduction in malpractice claims. Financially, the clinic saved over 3,000 staff hours annually, which translated into cost savings of approximately $500,000 within the first year17.
Challenges: Initial resistance from staff was a key hurdle, particularly due to concerns about the complexity of the system. The clinic addressed this by investing heavily in user training and customization, ensuring the EHR aligned with clinicians’ workflows.
2. King Abdulaziz Medical City (KAMC) EHR Implementation
In Saudi Arabia, King Abdulaziz Medical City (KAMC) successfully implemented a large-scale EHR system across its five campuses, despite facing delays due to the Middle East Respiratory Syndrome (MERS-CoV) outbreak.
The implementation, which focused on leadership engagement and extensive staff training, allowed the hospital to meet Joint Commission International (JCI) standards and drastically improve patient care. After the EHR rollout, KAMC saw a 20% increase in patient throughput and saved approximately 10% on overtime costs through better workflow management18.
Challenges: The outbreak of MERS-CoV disrupted the timeline, but the leadership’s flexibility in adjusting training schedules ensured the project was completed on time. The hospital’s robust change management process played a key role in overcoming delays.
3. Mental Health Hospitals in England
The implementation of modern EHR systems in mental health hospitals across England transformed long-term patient care. These facilities traditionally relied on paper-based records, making the management of complex patient data inefficient.
The integration of EHR systems allowed for improved collaboration among providers, enhanced data accessibility and reduced clinical errors. Over a three-year period, the hospitals experienced a 40% reduction in medical errors and a 30% improvement in care continuity, directly benefiting both patients and staff19.
Challenges: One of the main challenges was integrating narrative-based records typically used in mental health care into a digital format. The solution was to customize the EHR to support narrative entries, enabling seamless transitions from paper to digital.
Conclusion
In this blog, we’ve explored how effective healthcare project management—through EHR implementations, compliance strategies, and performance tracking—can lead to significant improvements in patient care, operational efficiency, and cost savings.
To manage these complex projects and ensure regulatory compliance, project managers need tools designed specifically for the healthcare industry.
Mirorim is the only productivity-first project management software that offers everything you need to streamline your operations. With features like custom dashboards for performance monitoring, and collaboration tools tailored for healthcare teams, Mirorim helps you easily stay on top of your projects.
Start your free trial today and experience how Mirorim can transform your healthcare projects. Don’t wait—join the growing number of healthcare leaders already driving better patient outcomes and achieving regulatory compliance with Mirorim. Create Your Free Account Now!
References
- Apra. (2021, October 14). The Hidden Epidemic – Preventable medical errors. APRA. https://www.americanpatient.org/the-hidden-epidemic-preventable-medical-errors/ ↩︎
- The high cost of botched EHR implementations. (n.d.). https://www.healthitoutcomes.com/doc/the-high-cost-of-botched-ehr-implementations-0001 ↩︎
- Larson, R. & Larson, E. (2009). Top five causes of scope creep … and what to do about them. Paper presented at PMI® Global Congress 2009—North America, Orlando, FL. Newtown Square, PA: Project Management Institute. https://www.pmi.org/learning/library/top-five-causes-scope-creep-6675 ↩︎
- “Mastering Cost Overrun: Strategies, Techniques, and Real-Life Examples for Effective Project Management” – PMI BIS Consultancy. (n.d.). https://pmiuk.co.uk/mastering-cost-overrun-strategies-techniques-and-real-life-examples-for-effective-project-management/ ↩︎
- A primer on project management for health care. (2023, October 20). Executive and Continuing Education. https://www.hsph.harvard.edu/ecpe/a-primer-on-project-management-for-health-care/ ↩︎
- Rudder, A. (2024, June 2). Scope creep: Definition, examples & how to Prevent it. Forbes Advisor. https://www.forbes.com/advisor/business/scope-creep/ ↩︎
- Nguyen, P. T. L., Phan, T. a. T., Vo, V. B. N., Ngo, N. T. N., Nguyen, H. T., Phung, T. L., Kieu, M. T. T., Nguyen, T. H., & Duong, K. N. C. (2024). Medication errors in emergency departments: a systematic review and meta-analysis of prevalence and severity. International Journal of Clinical Pharmacy. https://doi.org/10.1007/s11096-024-01742-w ↩︎
- Regulatory Overload Report | AHA. (2017, November 3). American Hospital Association. https://www.aha.org/guidesreports/2017-11-03-regulatory-overload-report ↩︎
- ProjectPractical. (2024, June 25). Effective strategies for quality audits in project management. ProjectPractical.com. https://www.projectpractical.com/quality-audit-in-project-management/ ↩︎
- Wolford, B. (2023, September 14). What are the GDPR Fines? GDPR.eu. https://gdpr.eu/fines/ ↩︎
- Berger, S., Saut, A. M., & Berssaneti, F. T. (2020). Using patient feedback to drive quality improvement in hospitals: a qualitative study. BMJ Open, 10(10), e037641. https://doi.org/10.1136/bmjopen-2020-037641 ↩︎
- A study of hybrid-agile: Agile with discipline at IBM. (n.d.). https://scds.cdm.depaul.edu/wp-content/uploads/2017/05/SOCRS_2017_paper_16.pdf
↩︎ - Fister Gale, S. (2018). Under Lock and Key: There’s Mounting Pressure to Ensure Data Safety; but Project Teams Must Manage Risk and New Requirements. PM Network, 32(10), 54–61. https://www.pmi.org/learning/library/project-teams-risk-management-data-privacy-11397 ↩︎
- Steve Alder on Mar 4, 2024, Healthcare Experiences More Third-Party Data Breaches Than Any Other Sector https://www.hipaajournal.com/healthcare-highest-third-party-breaches/ ↩︎
- Mph, J. H. (2023, September 6). The Ultimate Guide to Medical Office HIPAA Compliance. The Fox Group. https://www.foxgrp.com/hipaa-compliance/the-ultimate-guide-to-medical-office-hipaa-compliance/ ↩︎
- Case study: “Impossible” data breach response for hospital network. (n.d.). https://www.canopyco.io/resources/hospital-phi-breach-case-study ↩︎
- Takian, A., Sheikh, A., & Barber, N. (2012). We are bitter, but we are better off: case study of the implementation of an electronic health record system into a mental health hospital in England. BMC Health Services Research, 12(1). https://doi.org/10.1186/1472-6963-12-484 ↩︎
- Takian, A., Sheikh, A., & Barber, N. (2012b). We are bitter, but we are better off: case study of the implementation of an electronic health record system into a mental health hospital in England. BMC Health Services Research, 12(1). https://doi.org/10.1186/1472-6963-12-484 ↩︎
- Takian, A., Sheikh, A., & Barber, N. (2012c). We are bitter, but we are better off: case study of the implementation of an electronic health record system into a mental health hospital in England. BMC Health Services Research, 12(1). https://doi.org/10.1186/1472-6963-12-484 ↩︎

